Robert Kollmorgen, DO, a UCSF Fresno orthopaedic surgeon, knew there had to be a safer and better alternative for arthroscopic surgery than placing a large post between a patient’s legs that places undue pressure on the groin.
In traditional hip arthroscopy, the surgeon places the post to pull the hip joint out of the socket so a small incision can be made to insert a tiny camera, called an arthroscope. The camera allows the surgeon to view structures of the hip joint on a video monitor.
But the traditional method may cause nerve injury to the groin in up to four percent of patients. Dr. Kollmorgen, who specializes in hip preservation and who has performed hip arthroscopy for 10 years, felt the odds of a patient having numbness (albeit usually temporary) post-surgery was too high. For more than a year, he has performed hip arthroscopy using a post-free technique that he developed and researched in partnership with three other hip preservation programs.
Dr. Kollmorgen now uses a pink pad positioning device that eliminates the need for a post to achieve hip distraction. Dr. Kollmorgen, who operates at Clovis Community Medical Center, is the only hip preservationist using the technique in the central San Joaquin Valley.
Three other surgeons across the United States also used the pink pad technique as part of the research. A total of 300 patients had the new post-free distraction for hip arthroscopy performed by the four surgeons without complication. Dr. Kollmorgen presented findings at an international meeting in Melbourne, Australia in October. The study has appeared in “The Journal of Arthroscopic and Related Surgery.”
Dr. Kollmorgen said the new technique has been used in more than 1,000 surgeries. It could revolutionize hip arthroscopy which is the fastest growing arthroscopic surgery in the country, he said. “There’s just some remarkable things we’re seeing since we’ve changed the way we’re doing hip arthroscopy. And I think it’s only going to get better as we keep refining our technique.”
The pink pad positioning device can save hospitals money by allowing surgeons to use an existing arthroscopic surgery table instead of a postless table that can cost as much as $80,000. And the benefits to patients are many.
“We’ve devised a technique to make it safer to patients. We’re decreasing complications; we’re making it so patients can recover quicker, have a better surgical experience.” Dr. Kollmorgen said. “Patients have reported less after-surgery pain. Our narcotic use after this operation is 10 pills on average.”
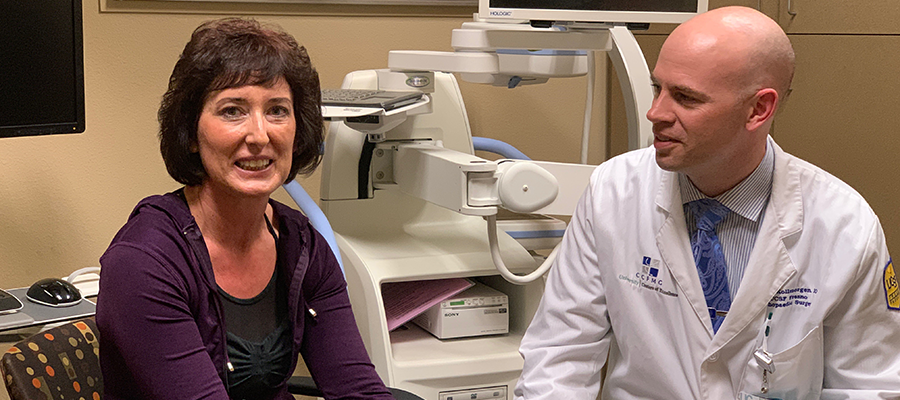
Maria Carr said she had a pain of eight on a scale of 10 in both hips last year before Dr. Kollmorgen performed revision hip arthroscopy surgery on her left hip on Oct. 29 and on the right on Dec. 31. After each surgery, Carr said she took only one pain pill on her first day at home post-surgery.
Carr, a director of special education, began physical therapy two weeks after each surgery. By mid-March, she said her recovery was going smoothly. “I was telling everyone I walked five miles’ yesterday in Santa Cruz in the rain and enjoyed a beautiful sunset. And the night before that I was at a yoga class.”
And Carr expects she will have another accomplishment to report soon. “My goal is to go hiking at Lake Tahoe in July.”
Carr almost had hip surgery by a Los Angeles surgeon who performed arthroscopic surgery on her hips 10 years ago. He wanted to do hip replacements, but Carr was reluctant. She heard about Dr. Kollmorgen from a physical therapist, sought his opinion and is glad she did. “Dr. Kollmorgen is amazing,” she said.
Patients need not go out of the Fresno area for the latest techniques in hip arthroscopy, Dr. Kollmorgen said. “We need people to know we’re here. Somehow we need to get the word out that we’re doing great things here. Research is here.”